Fåhræus–Lindqvist effect
- Should not be confused with "Fåhræus effect"
The Fåhræus–Lindqvist effect /fɑːˈreɪ.əs ˈlɪndkvɪst/[1] is an effect where the viscosity of a fluid, in this case blood, changes with the diameter of the tube it travels through; in particular there's a decrease of viscosity as the tube's diameter decreases (only if the vessel diameter is between 10 and 300 micrometers). This is because erythrocytes move over the center of the vessel, leaving plasma at the wall of the vessel.
Contents |
History
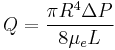
The effect is named after Swedish scientists Robin Fåhræus and Torsten Lindqvist. Robert (Robin) Sanno Fåhræus was a Swedish pathologist and hematologist, born on October 15, 1888, in Stockholm. He died on September 18, 1968, in Uppsala, Sweden. Johan Torsten Lindqvist is a Swedish physician, who was born in 1906.[2] Fåhræus and Lindqvist published an article in the American Journal of Physiology in 1931 describing the effect.[3] Their study represented an important advance in the understanding of hemodynamics which had widespread implications for the study of human physiology. They forced blood through fine glass capillary tubes connecting two reservoirs. Capillary diameters were less than 250 μm, and experiments were conducted at sufficiently high shear rates (≥100 1/s) so that a similar flow in a large tube would be effectively Newtonian. After correcting for entrance effects, they presented their data in terms of an effective viscosity, derived from fitting measured pressure drop and volume flow rate to Hagen–Poiseuille equation for a tube of radius R
where:
 is the volumetric flow rate
is the volumetric flow rate is the pressure drop across the capillary
is the pressure drop across the capillary is the length of capillary
is the length of capillary is the effective viscosity
is the effective viscosity is the radius
is the radius is the mathematical constant
is the mathematical constant
Although Hagen–Poiseuille equation is only valid for a Newtonian fluid, fitting experimental data to this equation provides a convenient method of characterizing flow resistance by a single number, namely  . In general,
. In general,  will depend on the fluid being tested, the capillary diameter, and the flow rate (or pressure drop). However, for a given fluid and a fixed pressure drop, data can be compared between capillaries of differing diameter.[4] Fahraeus and Lindqvist noticed two unusual features of their data. First,
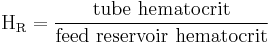
will depend on the fluid being tested, the capillary diameter, and the flow rate (or pressure drop). However, for a given fluid and a fixed pressure drop, data can be compared between capillaries of differing diameter.[4] Fahraeus and Lindqvist noticed two unusual features of their data. First,  decreased with decreasing capillary radius, R. This decrease was most pronounced for capillary diameters < 0.5mm. Second, the tube hematocrit (i.e., the average hematocrit in the capillary) was always less than the hematocrit in the feed reservoir. The ratio of these two hematocrits, the tube relative hematocrit,
decreased with decreasing capillary radius, R. This decrease was most pronounced for capillary diameters < 0.5mm. Second, the tube hematocrit (i.e., the average hematocrit in the capillary) was always less than the hematocrit in the feed reservoir. The ratio of these two hematocrits, the tube relative hematocrit,  ,is defined as
,is defined as
Explanation of phenomena
These initially confusing results can be explained by the concept of a plasma cell-free layer, a thin layer adjacent to the capillary wall that is depleted of red blood cells. Because the cell-free layer is red cell-poor, its effective viscosity is lower than that of whole blood. This layer therefore acts to reduce flow resistance within the capillary, with the net effect that the effective viscosity is less than that for whole blood. Because the cell-free layer is very thin (approximately 3 μm) this effect is insignificant in capillaries whose diameter is large. This explanation, while accurate, is ultimately unsatisfying, since it fails to answer the fundamental question of why a plasma cell-free layer exists. There are actually two factors which promote cell-free layer formation.
- For deformable particles (such as red blood cells) flowing in a tube, there is a net hydrodynamic force that tends to force the particles towards the center of the capillary. This is known as the Segre–Silberberg effect.
- It is clear that red blood cells cannot pass through the capillary wall, which implies that the centers of red blood cells must lie at least one red blood cell half-thickness away from the wall. This means that, on average, there will be more red blood cells near the center of the capillary than very near the wall.
Cell-free marginal layer model is a mathematical model which tries to explain Fåhræus–Lindqvist effect mathematically.
Further reading
- Schmidt, Lang (Hrsg.): Physiologie des Menschen: Mit Pathophysiologie (S. 623). Springer, Berlin; 30. Auflage 2007. ISBN 978-3540329084
- This article incorporates information from the German Wikipedia.
See also
References
- ^ [1]
- ^ Lee Waite, Jerry Fine (2007). Applied biofluid mechanics. New York: McGraw-Hill. ISBN 0071472177. http://www.amazon.com/Applied-Biofluid-Mechanics-Lee-Waite/dp/0071472177.
- ^ Fahraeus R, Lindqvist T (1931) The viscosity of the blood in narrow capillary tubes. The American Journal of Physiology 96:562–568.
- ^ Ethier, C. Ross; Simmons, Craig A. (2007). Introductory biomechanics : from cells to organisms (Repr. with corrections ed.). Cambridge [u.a.]: Cambridge Univ. Press. ISBN 0521841127. http://www.amazon.com/Introductory-Biomechanics-Organisms-Biomedical-Engineering/dp/0521841127.